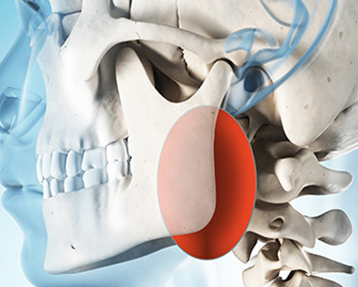
Thyroid Tumor
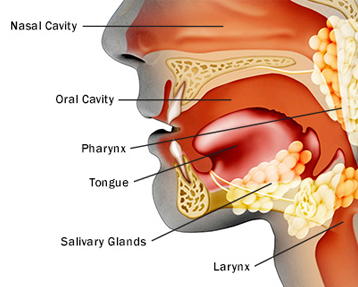
The thyroid is part of the body’s endocrine system, a system of glands that control hormones in the body. It normally weighs less than an ounce, and it cannot be seen or felt in most people; however it has an important function. The thyroid makes hormones that help regulate the body’s heart rate, blood pressure, temperature and metabolism (the breakdown of food to create energy).
Thyroid gland cells are the only cells in the body that absorb and retain iodine. Iodine is needed to make thyroid hormones.
Two kinds of cells are found in the thyroid
- Follicular cells are the most common. They produce thyroid hormone, which is important for growth; mental function and helping the body create energy.
- Parafollicular cells (also known as C cells) produce a small amount of the hormone calcitonin, which has a minor role to control calcium metabolism. Most parafollicular cells are in the upper third of each lobe.It is a disease in which cells grow abnormally and have the potential to spread to other parts of the body. Risk factors include radiation exposure at a young age, having an enlarged thyroid, and family history
Types of Thyroid Cancer
- Papillary Thyroid Cancer: Papillary Thyroid Cancer is the most common type of thyroid cancer, accounting for about 80% of thyroid cancers. While papillary thyroid cancer typically occurs in only one lobe of the thyroid gland, it may arise in both lobes in up to 10% to 20% of cases. Papillary thyroid cancer is most common in women of childbearing age. It sometimes is caused by exposure to radiation.
Even though papillary thyroid cancer is usually not an aggressive type of cancer, it often metastasizes (spreads) to the lymph nodes in the neck. Papillary thyroid cancer treatment usually is successful. - Follicular Thyroid Cancer: Follicular thyroid cancer accounts for about 10% of thyroid cancers. Like papillary thyroid cancer, follicular thyroid cancer usually grows slowly. Its outlook is similar to papillary cancer, and its treatment is the same.This kind of thyroid cancer usually stays in the thyroid gland but sometimes spreads to other parts of the body, such as the lungs or bone. However, it usually does not spread to lymph nodes. It is more common in countries where diets do not contain enough iodine.Hurthle cell carcinoma, also called oxyphil cell carcinoma, is a type of follicular thyroid cancer. Most patients diagnosed with Hurthle cell cancer do well, but the outlook may change based on the extent of disease at the time of diagnosis.Follicular thyroid cancer
- Medullary Thyroid Cancer: MTC is the only type of thyroid cancer that develops in the parafollicular cells of the thyroid gland. It accounts for 3% to 10% of thyroid cancers. Medullary thyroid cancer cells usually make and release into the blood proteins called calcitonin and/or carcinoembryonic antigen, which can be measured and used to follow the response to treatment for the disease. Sometimes medullary thyroid cancer spreads to the lymph nodes, lungs or liver before a nodule is found or the patient has symptoms. MTC can be treated more successfully if it is diagnosed before it has spread.
There are two types of MTC:
- Sporadic MTC is more common, accounting for 85% of medullary thyroid cancers. It is found mostly in older adults and is not inherited.
- Familial MTC is inherited, and it often develops in childhood or early adulthood. If familial MTC occurs with tumors of certain other endocrine organs (parathyroid and adrenal glands), it is called multiple endocrine neoplasia type 2 (MEN 2). If you have a family history of MTC, it is important for you and your children to be tested for the gene that causes the disease.
- Anaplastic Thyroid Cancer:Anaplastic thyroid cancer is the most dangerous form of thyroid cancer. It is makes up only 1% of thyroid cancers. It is believed that anaplastic thyroid cancer grows from a papillary or follicular tumor that mutates further to this aggressive form. Anaplastic thyroid cancer spreads rapidly into areas such as the trachea, often causing breathing difficulties. Anaplastic thyroid cancer sometimes is called undifferentiated thyroid cancer because the cells are so different from normal thyroid tissue.
Causes of Thyroid Cancer
Environmental exposure to ionizing radiation from both natural background sources and artificial sources is suspected to play a significant role, and there are significant increased rates of thyroid cancer in those exposed to mantlefield radiation for lymphoma, and those exposed to iodine-131. Thyroiditis and other thyroid diseases also predispose to thyroid cancer.Inherited disorders also play a role in Familial medullary thyroid cancer, which is usually caused by an inherited mutation in the RET gene. If your parent has the gene mutation, you have a 50% chance of having it too. If you inherit the gene, you are likely to develop the cancer. Other types of thyroid cancer also may be caused by diseases that run in families.Iodine deficiency is found to be one more cause of Thyroid Cancer.
Signs and Symptoms
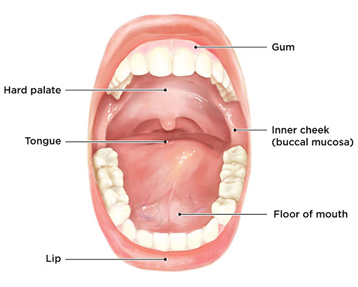
- A nodule in the thyroid region of the neck
- An enlarged lymph node
- pain in the anterior region
- Breathing problems, especially the feeling that you are breathing through a straw
- Cough that does not go away and is not caused by a cold
- Swallowing problems
- Cough with blood
- Changes in voice due to an involvement of the recurrent laryngeal nerve.
Thyroid Cancer Diagnosis
One or more of the following tests may be used to find out if you have cancer and if it has spread. These tests also may be used to find out if treatment is working.
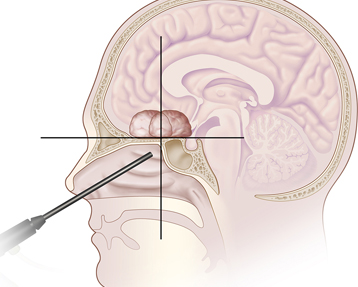
- Fine-needle aspiration biopsy (FNA) : Biopsy (removal of a small number of cells and looking at them under a microscope) is the only way to tell for sure if you have thyroid cancer. In FNA, a thin needle is inserted into the nodule, and cells are taken out to biopsy. Most thyroid nodules are proved by FNA to be benign (not cancer). If the FNA is inconclusive (not showing clearly if the nodule is cancerous), more testing may be needed.
- Ultrasound
- CT or CAT (computed axial tomography) scans
- MRI (magnetic resonance imaging) scans
- PET (positron emission tomography) scans
- Radioactive thyroid scan: If a nodule is papillary or follicular cancer, a radioactive thyroid scan may be used after thyroid surgery to determine if cancer remains or has spread to other parts of the body. Medullary thyroid cancer cells don’t absorb iodine, so this test is not useful in this type of thyroid cancer.
- Blood tests
- Genetic testing: If you have medullary thyroid cancer, you will be given a blood test to determine if you carry a gene that sometimes causes this cancer. If the test is positive, your children and parents should be tested to see if they have the gene or thyroid cancer. More than 90% of people who have the gene will eventually develop thyroid cancer.
If your child has the gene, the doctor probably will suggest removal of the thyroid. Although children rarely develop cancer before 5 years old, one type of MTC known as MEN-2B can develop in the early months of life. If the thyroid is removed, then that person will take daily thyroid medication for the rest of his or her life.
Some cases of thyroid cancer can be passed down from one generation to the next. Genetic counselling may be right for you. Learn more about the risk to you and your family on our genetic testing page.
Treatment
Scarless or Minimally invasive Thyroidectomy:This procedure is meant to perform half or total removal of thyroid gland by a technique which causes fewer scars in the neck or no visible scar in the neck.
Indications
There should be no previous surgeries in the same area of neck with nodule or thyroid size <=5cm, larger thyroid can also be removed with no visible scar but with combined approach (placing incision in the skin behind the ear and in the armpit)
Technique
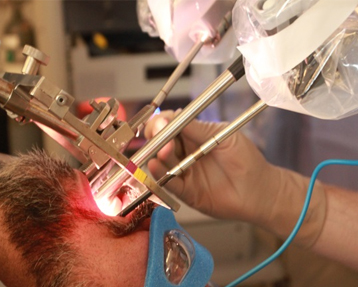
Retroauricular approach in which incision is placed in area behind the ear and in the hairline so it is not visible, tunnel is created up to the thyroid lobe which is to be removed. The skin flap is held up with Chung’s retractor. Endoscope is introduced with for magnified view, specialised instruments are used to perform thyroidectomy (half or total removal of thyroid gland). Incision on other side may be required for removal of opposite thyroid. Special care is taken during surgery for identification of recurrent laryngeal nerve and its preservation, so that injury to this nerve is avoided. Parathyroid glands which are situated on the backside of thyroid lobe, control level of calcium in the body. These glands need to be preserved so that calcium levels are maintained in normal. For the utmost care during surgery we prefer ROBOTIC SURGERY (DAVINCI – XI) or ENDOSCOPIC SURGERY. Endoscopic surgery comes with the advantage of same approach with much decreased cost
There are three main risks for total thyroidectomy.
- Recurrent laryngeal nerve injury : This nerve controls your vocal cords and if injured you will have a hoarse voice. There is a 1% chance of permanent hoarseness and a 5% chance of temporary hoarseness (<6months).
- Low blood calcium :There are parathyroid glands that lie behind your thyroid gland that help to control your blood calcium levels. If they are injured or removed (can lie within the thyroid gland) during your operation, then your blood calcium can be too low. This would require you to take calcium and vitamin D supplementation. There is a 1% chance of permanent calcium supplementation and 5% chance of temporary calcium supplementation.
- Bleeding : There is a 1/300 risk of bleeding with your operation. This is the main reason you stay overnight in the hospital.
Prognosis
Admission in the hospital is for 1-2 days. Recovery time is 2weeks. Endoscopic neck dissection (surgery) is a technically feasible and safe technique for treating early-stage thyroid cancer.